Study Suggests Side-Effects and Costs Are Biggest Issues for Users of HIV Pre-Exposure Prophylaxis
Respondents preferred long-acting injectable PrEP, which came to market in early 2022, over short-acting pills

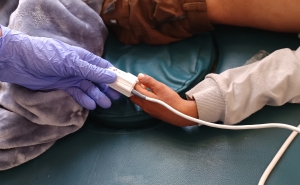
A new survey finds that men who would be potential users of HIV pre-exposure prophylaxis (PrEP) medication prefer long-acting injections over pills, but rank side effects and costs as the most important issues for them in considering whether to take PrEP. The study, published online January 21 in AIDS and Behavior, was co-led by researchers at the Johns Hopkins Bloomberg School of Public Health. Unlike previous studies, the survey took into account the multiple factors that people consider when making a decision to take PrEP: cost, side effects, travel time, and pills versus injections.
HIV PrEP came to market in 2012 after the Food and Drug Administration approved a once-daily pill that requires monthly check-ins. The FDA approved a long-acting injectable PrEP in December 2021. Heralded as a critical prevention tool, PrEP proved to be 99 percent effective in blocking HIV infection when used correctly. However, uptake has been slow. As of 2020, only about 25 percent of people for whom PrEP is recommended were using it, according to the Centers for Disease Control and Prevention, with uptake among Black and Hispanic people estimated at only 9 and 16 percent, respectively, in 2020.
An initiative led by the U.S. Department of Health and Human Services, Ending the HIV Epidemic in the U.S., aims to increase overall PrEP uptake to 50 percent by 2030.
The survey, fielded from May 2020 through October 2021, examined preferences relating to PrEP in a sample of 688 gay, bisexual, and other men who have sex with men. The sample included people who had previously used PrEP as well as those who had not. Respondents tended to rank side effects as the most important factor, followed by costs. And although they preferred long-acting injection over other ways of taking PrEP, they ranked mode of administration as the least important issue.
“PrEP is very effective at preventing HIV transmission but has relatively low uptake; our results suggest that public health policymakers might be able to boost PrEP uptake by keeping costs low, and if health care practitioners communicate clearly about the potential PrEP side effects, regardless of what type of PrEP they decide to take,” says study co-first author Lorraine T. Dean, ScD, associate professor in the Bloomberg School’s Department of Epidemiology.
Dean’s co-first author on the paper was Zachary Predmore, PhD, associate policy researcher at the RAND Corporation. Predmore conducted the research while he was completing his PhD at the Bloomberg School.
The researchers recruited participants to the study by advertising on social media between May 2020 and October 2021. Participants were asked to fill out an online survey known as a discrete choice experiment—designed to reveal not only the participants’ real-world preferences but also the relative strengths of those preferences.
The results indicated that the participants, in considering whether to take PrEP, regarded potential side effects as most important. On average they would have preferred to pay $200—the highest cost in the choices offered—for PrEP with no side effects, rather than paying nothing for PrEP with long-term side effects.
Nausea, vomiting and other gastrointestinal problems are potential side effects of PrEP, but have been reported by only a small percentage of people taking these medications.
Second and third in importance to study participants were out-of-pocket PrEP costs, and travel time for follow-up medical visits. The new injectable PrEP starts with a monthly injection for two months, then one injection every two months. In contrast, PrEP pills are typically prescribed to be taken once daily. People taking the medication are monitored in person every 90 days or four times a year, while those using injectables get checked every two months, approximately six times per year.
Respondents considered mode of administration the least important factor, although their preference on the whole was for a long-acting injected version over a daily pill or an as-needed short course of pills.
Subgroup analyses indicated that those making less than $75,000 per year and those with prior experience taking PrEP tended to have stronger preferences for lower-cost PrEP.
The results underscore the need to keep PrEP money and time costs, as well as side-effects, low in order to improve uptake, Dean says.
Although the U.S. Preventive Services Task Force gave PrEP an “A” rating in 2019—effectively making PrEP and associated clinical services available at low or no cost under Affordable Care Act-compliant health insurance policies—not everyone who needs PrEP is covered by such policies, or by any health insurance at all.
“I hope our results will encourage non-ACA insurers to keep PrEP at zero cost to those who need it,” Dean says. “Ideally, injectable PrEP needs to be fast, free, and have minimal side effects, and our results suggest that could really be said about all PrEP products.”
She and her colleagues are now following up the study with an analysis of PrEP preferences by race and other demographic groupings.
“Optimizing uptake of long-acting injectable pre-exposure prophylaxis for HIV prevention for men who have sex with men” was written by Lorraine Dean, Zachary Predmore, Alexandra Skinner, Siena Napoleon, Philip Chan, and Julia Raifman.
The research was supported by the National Institutes of Health (R21 MH118019-01).
# # #
Media contacts: Jonathan Eichberger at je@jhu.edu and Kristine Henry at khenry39@jhu.edu.