Hepatitis B Vaccination is an Essential Safety Net for Newborns
Without vaccination, as many as 9 in 10 infants infected with hepatitis B in their first year of life will develop chronic infection that can lead to liver failure and death.

Since 1991, when the CDC and the American Academy of Pediatrics recommended hepatitis B vaccination for all newborns, infections with hepatitis B virus in children and teens have decreased by 99%.
Newborns, infants, and young children are particularly susceptible to hepatitis B and more likely than teens and adults to develop chronic infection that leads to life-threatening complications, including cirrhosis and liver cancer. And of those who develop chronic hepatitis B infection, 15%–25% will die from the disease.
“From a public health perspective, universal hepatitis B vaccination at birth has been extremely effective in reducing infections and is the best strategy to minimize the risk of transmission to all infants,” says William Moss, MD, MPH, a professor in Epidemiology and executive director of the International Vaccine Access Center.
What is Hepatitis B?
Hepatitis B virus is an extremely contagious virus that infects the liver. It is the leading cause of liver cancer worldwide. Hepatitis B virus can cause both acute infection—which lasts several weeks and can entail severe symptoms—and chronic infection, which can last a lifetime. The most recent CDC data estimates that about 640,000 adults in the U.S. have chronic hepatitis B.
Infection does not cause symptoms immediately. Acute infection can take up to six months for symptoms to present, which can range from mild to severe. “Many hepatitis B virus infections—both acute and chronic—are without symptoms, until a person with chronic infection develops the signs and symptoms of liver failure or cancer,” Moss says. “As many as half of all people infected with the virus may not be aware of their infection” and thus risk unknowingly transmitting the virus to others.
Hepatitis B Risk in Newborns and Children
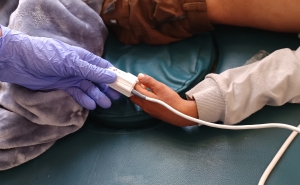
Hepatitis B virus is transmitted through blood and bodily fluids—even in microscopic amounts—and the virus can survive on surfaces for up to a week. It can be transmitted sexually or through contaminated needles, but globally one of the most common transmission routes is during birth from an infected mother.
In addition to perinatal transmission, the American Academy of Pediatrics explains that the virus can also be transmitted through close contact—with minor cuts or even microscopic amounts of blood on a shared surface, for example—to an infant by a caregiver or household member with an infection, even when the infected person is asymptomatic. This is why testing and vaccination for hepatitis B are also recommended for all family members and people sharing a home with an infant.
An infant infected with hepatitis B is unlikely to show symptoms of an acute infection, Moss explains, but they are highly likely to develop chronic infection. “As many as 90% of infants infected around birth or in the first year of life will develop chronic infection, compared to only 5%–10% of older children and adults,” he says.
In 1991, the Advisory Committee for Immunization Practices recommended hepatitis B vaccination at birth for all newborns. Within 10 years of the universal birth dose recommendation being in place, hepatitis B cases among U.S. children ages 6–19 dropped by 68%.
“Universal hepatitis B vaccination at birth has nearly eliminated perinatal hepatitis B virus transmission in the United States,” says Moss. “It’s a remarkable accomplishment that has prevented many cases of cirrhosis, liver cancer, and death.”
The Childhood Hepatitis B Vaccine Series is Extremely Effective
The hepatitis B vaccine is delivered as a 3–4-dose series. For most children in the U.S., the series begins at birth and is completed by 15 months of age. When given within 24 hours of birth, the vaccine is up to 90% effective in preventing perinatal infection.
After completing the course, 98% of healthy infants achieve full immunity that lasts at least 30 years. When the vaccine series is started at birth, it has shown to reduce a person's risk of liver cancer by 84% and death from liver disease by 70%.
Hepatitis B Vaccination Has an Excellent Safety Record
As with any vaccine, the CDC monitors the safety of the hepatitis B vaccine and has repeatedly found it to be extremely safe. Study after study have shown the vaccine is not associated with an increased risk of infant death, fever or sepsis, multiple sclerosis, or autoimmune conditions, and severe reactions are rare.
“There is no evidence to suggest that hepatitis B vaccination at birth is risky compared to the benefits it offers, particularly given the high risk of chronic infection in unvaccinated infants exposed to the virus,” Moss says.
The Role of Maternal Testing for Hepatitis B
Since 1988, the CDC has recommended hepatitis B testing during pregnancy, with the most recent guidance specifying the first trimester as the preferred timing. A mother’s hepatitis B status—whether positive, negative, or unknown—informs the timing of the birth dose and whether hepatitis B immune globulin is also administered.
However, a negative test result during pregnancy does not guarantee the child will not be infected with hepatitis B virus. In addition to the potential for false negative test results, “the mother could acquire hepatitis B virus infection after testing, thus the risk is not zero,” Moss explains.
Additionally, many pregnant people do not get the recommended testing or treatment. Every year, approximately 14% of pregnant mothers do not receive testing, and of mothers who test positive, more than half do not receive the recommended monitoring tests during pregnancy and after delivery.
More from the Bloomberg School
- See latest headlines
- Learn more about our departments: