2023-24 Year In Review
The Right Place
I often tell my students, “if you want to change the world, you’re in the right place.” Our first-ever HPM Year-in-Review, highlighting just a few of our many accomplishments, proves that true. Every day, HPM students, faculty, staff and alumni are producing new evidence and analysis, leading to health policy changes that will improve lives across the country.
Our success is due in part to our growth. Since I became chair in February 2022, we increased the size of the department by 47%. Critically, we increased not only the number in our ranks, but also the diversity. New faculty—including some HPM alums—represent a wide range of identities and brought expertise in health care economics, LGBTQ health issues, mental health, gun violence, family caregiving policy and more. New staff were likewise diverse and brought a wealth of skills from grants management and budget analysis to public relations and digital marketing.
I am incredibly proud of this growth, which sets the stage for an even brighter future. On the horizon is a new building, more opportunities at the Johns Hopkins Bloomberg Center in Washington, DC, and an influx of scholarship funding that will enable us to welcome more first generation and limited income students to the MSPH in Health Policy program.
I hope you will join me in celebrating all of the great, world-changing work of the 2023 – 2024 academic year and all that is to come. We are in the right place.

HIGHLIGHTS
#1
health policy and management program in the country as voted on by peers in the 2024 - 2025 U.S. News & World Report Graduate School report
247
diverse faculty & staff
300+
outstanding students
$500K+
in scholarships prioritizing first generation, limited-income and/or students from underrepresented groups.
OUR WORK
Every day, the Department of Health Policy & Management advances evidence-informed solutions to public health challenges and trains the next generation of leading health administrators, advocates, policymakers and researchers. Our work can be understood as three distinct, equally important areas of focus:
- Insights, which encompasses the high-quality, thought-provoking data and analysis disseminated by HPM faculty and students.
- Impact, which includes noticeable shifts in policy discussions and tangible policy changes informed and effected by our work
- Community, in which we recognize the rich diversity of perspectives among HPM students, faculty, staff and alumni and nurture a sense of belonging and shared purpose.
In our 2023 – 2024 Year in Review, we proudly spotlight stand-out examples of HPM in action:
INSIGHTS
Sparking Dialogue & Scalable Solutions at Convenings
Four years after the pandemic began, there’s increasing demand for in-person convenings that not only disseminate information but offer opportunities for organic enlightening conversations. In the 2023 – 2024 academic year, HPM hosted a wide range of events at the Johns Hopkins Bloomberg Center in Washington, DC, including:

Spotlighting Health Disparities
From December 2023 – June 2024, Johns Hopkins Center for Health Disparities Solutions, led by Professor Darrell Gaskin, PhD hosted four HOPE Challenge events addressing critical racial and ethnic health disparities in the United States. These included HIV and the Politics of Race (December 1, 2023); Cardiovascular Health Disparities (February 6, 2024); Black Maternal and Infant Health (May 24, 2024); and Gun Violence Prevention in Communities of Color (June 4, 2024). Attended by 1,000+ policymakers, researchers, advocates, and community leaders, HOPE Challenge events proposed actionable policy recommendations, including expanding Medicaid coverage, addressing social determinants of health, improving data collection, increasing healthcare provider diversity, and leveraging technology for better health outcomes. Among the distinguished speakers were Congresswoman Maxine Waters (HIV and the Politics of Race), Congresswoman Lauren Underwood (Black Maternal and Infant Health), and Reverend Al Sharpton (Gun Violence Prevention in Communities of Color).
Integrating Health in All Policies
On Friday, May 10, the Institute for Health and Social Policy, led by Chair Keshia Pollack Porter, PhD, MPH, held a first-of-its-kind convening, Health in All Policies: Innovative Tools to Integrate Health and Equity Into All Policymaking. Hosted in partnership with SOPHIA and AcademyHealth, the event explored how non-health policies across sectors—including housing, education, employment and the environment—can be assessed and shaped by their potential impacts on health and equity. Attendees from across the country gathered to share concrete examples of policymaking informed by health impact and equity assessments. Maryland State Delegate Robbyn T. Lewis gave a fireside chat about her experience integrating health and equity in legislation and several policymakers and experts participated in a panel discussion and a series of lightning talks. Panelists included Jimmy Dills, Georgia Health Policy Center; Danaya Hough, District of Columbia Council Office of Racial Equity; Keshia Pollack Porter, PhD, MPH, Johns Hopkins Bloomberg School of Public Health; Elizabeth Ramey, Colorado General Assembly and moderator Kristin Rosengren, AcademyHealth.
The Environmental Impact of Health Care
In April, the Hopkins Business of Health Initiative, led by Professor Daniel E. Polsky, PhD, hosted an Earth Day event centered on mitigating the healthcare sector’s carbon footprint. Across the U.S., health care delivery requires single-use, often non-recyclable materials, all of which end up either incinerated or in landfills. As a result, the sector currently accounts for 8.5% of U.S.-produced greenhouse gas emissions. Secretary of Health & Human Services Secretary Xavier Becerra, who participated in a fireside chat at the event, declared that America's hospital systems and medical providers are collectively "the largest power plant in the nation." Following Becerra’s remarks, a panel of clinicians, including Women’s Health Nurse Practitioner Deanna Benner, ChristianaCare; Jeremy Greene, MD, Johns Hopkins School of Medicine; and Jodi Sherman, MD, Yale School of Medicine emphasized the importance of engaging frontline staff in sustainability initiatives, provided historical context for the shift toward disposable medical supplies and noted a need for standardized sustainability metrics and possible international collaboration to drive market changes. Panelists agreed that progress depends on collaboration between policymakers, providers, and the community and applauded Johns Hopkins for training the next generation of leaders in health care administration.
Shining a Light on the Mental Health Effects of the Dobbs Decision
In 2022, the Supreme Court overturned Roe v. Wade, which had ensured legal abortion and reproductive care access to women for nearly 50 years. In January 2024 a study by HPM PhD candidate Benjamin Thornburg, Assistant Professor Alene Kennedy-Hendricks, PhD, Professor Joanne Rosen, PhD and Associate Professor Matthew Eisenberg, PhD, Director of the Center for Mental Health and Addiction Policy in JAMA Network examined the impact of the Dobbs decision on mental health in states with trigger abortion bans that went into effect immediately following the decision. The study found anxiety and depression symptoms worsened in states with such bans and were most pronounced among females ages 18 to 45. The insights have proven valuable and timely, as states across the country continue to consider restricting or protecting abortion access and the issue remains at the forefront of the 2024 presidential election.

Defining the Impact of Youth Caregiving on Education and Opportunity
Family caregivers are often the primary providers of long-term care in the United States. A study published this year by Assistant Professor Katherine Miller, PhD shed light on the often-overlooked role of youth and young adults as caregivers in the United States. The study estimates that millions of young Americans between the ages of 15 and 22 are providing essential care to adults, significantly impacting those young peoples’ educational opportunities and achievements. The study reveals that an estimated 1.6 million youth (ages 15-18) and 2 million young adults (ages 19-22) are caregivers, representing 9.2% and 12.7% of their respective age groups. Youth caregivers are 8% less likely to be enrolled in school than non-caregiving peers, while those that are enrolled spend 44 minutes fewer minutes per day on education and work-related activities. Overall, the study demonstrates how caregiving may adversely impact young people’s short and long-term outcomes and serve as a structural barrier to wellbeing.

IMPACT
Substance Abuse Treatment Expands in Correctional Facilities
In a report from the Bloomberg American Health Initiative with support from the Bloomberg Overdose Prevention Initiative, Professor Brendan Saloner, PhD and Senior Practice Associate Sara Whaley, MPH, MSW, MA made recommendations to the federal government to expand access to methadone treatment in correctional facilities. The 2022 report argued that increasing availability of methadone to incarcerated persons could be a key intervention to preventing fentanyl- and other opioid-related overdose deaths and reducing recidivism. In 2024, after many ensuing conversations, the Substance Abuse & Mental Health Services Administration (SAMHSA) issued a final rule on methadone treatment in correctional facilities and rolled out federal initiatives to promote and increase access. More than 250 corrections administrators and policymakers attended a forum in March about the new guidelines. Rahul Gupta, Director of The White House's Office of National Drug Control Policy (ONDCP) emphasized the potential impact of this policy change in his opening remarks, saying “if every jail and prison across America offered treatment for [Opioid Use Disorder], we could save up to 16,000 lives from overdose deaths each year.”

Medicare Negotiates Drug Prices, Increasing Access & Affordability
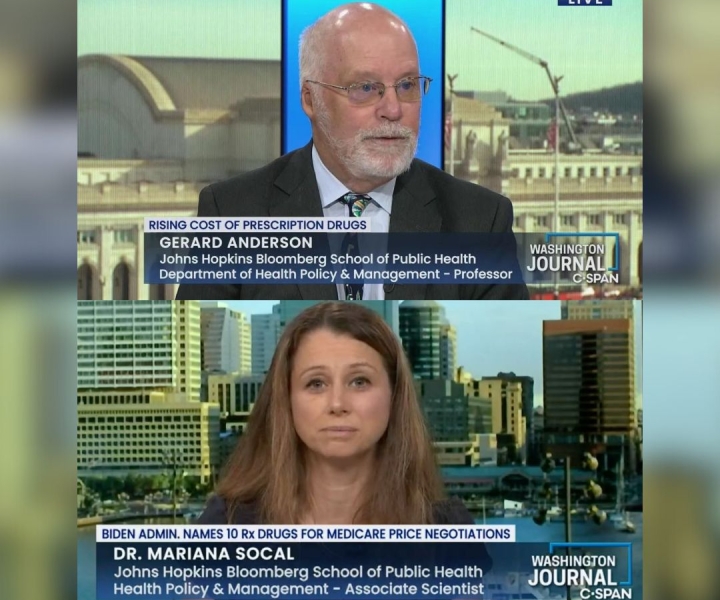
Professor Gerard Anderson, PhD helped draft the 2003 legislation that first created the Medicare prescription drug plan and as he told the Public Health on Call podcast in 2022, Congressional leaders had always hoped to create subsequent legislation allowing the government to negotiate drug prices. It wasn’t until recent passage of the Inflation Reduction Act (IRA), which Anderson also advised on, that that hope became reality. Beyond enabling price negotiation, the IRA also prevents drug companies from raising prices faster than the rate of inflation and caps out-of-pocket costs for Medicare-fee-for-service beneficiaries to $2,000 per year. In the 2023 – 2024 academic year, Anderson analyzed draft guidelines for operationalizing the new program, advocating for competitive standards for drugs to enter the Medicare negotiation process, addressing payment and pricing components, and defining negotiation factors and processes. Associate Professor Mariana Socal, MD also produced a slew of research in the 2023 – 2024 schoolyear that will inform Medicare drug price negotiations, identifying complex challenges in pharmaceutical supply chains that could impact pricing and strategies to negotiate pricing for gene and RNA therapies used to treat rare diseases.
COMMUNITY
Commemorating 50 Years of Management Education
HPM marked 50 years of training leading health care administrators and executives at a cocktail reception and dinner in April 2024. The evening kicked off with an illuminating lecture from John D. Halamka, MD, MS, president of the Mayo Clinic Platform on the impact of AI in healthcare. Afterward, faculty, students and alumni across the decades mingled with hors d’oeuvres and drinks in the Bloomberg School of Public Health foyer, networking across cohorts, snapping group photos and trading memories. At dinner, guests heard remarks from Department Chair Keshia Pollack Porter, PhD; DrPH Program Director Mark Bittle, DrPH; and class of 1998 alum Aileen Tinney, MHA, President & CEO of Keswick among others. Thank you to all who joined us to celebrate this monumental occasion!

Celebrating Diversity with Humans of HPM
Many undergrads come with a limited understanding of “public health” and “health policy,” potentially restricting the careers they consider and opportunities they pursue. In 2024, the department launched a new video series, Humans of HPM, to showcase the vast array of health policy topics and diversity of backgrounds and paths to public health and health policy within our community. Among the first faculty featured were Assistant Professor Mark Meiselbach, PhD; Associate Professor Matt Eisenberg, PhD; Assistant Professor Catherine Ettman, PhD; Assistant Professor Ellesse-Roselee Akré, PhD; and Professor Daniel Webster, ScD, MPH. Together, these faculty are working on issues as varied as the availability and affordability of healthcare; the lasting impact of COVID-19 on mental health and wealth in the U.S.; substance abuse treatment healthcare coverage; mental health challenges at the intersection of transgender status, race and ethnicity; and public health approaches to reducing gun violence. We look forward to profiling many more students, faculty, staff and alumni and their unique paths to HPM in the coming year!

