Preventing Cancer: The Far-Reaching Impact of Vaccines

For the past 25 years, the global health community has come together each February for World Cancer Day, a time to raise awareness about the impact of cancer and encourage evidence-based prevention strategies. One such strategy is immunization, as certain vaccines have been shown to effectively protect against cancer-causing viruses, including human papillomavirus (HPV) and hepatitis B virus (HBV). These vaccines have the potential to avert and even eliminate some types of cancers, making it all the more critical to ensure that children and adolescents everywhere receive access to these life-saving interventions.
HPV Vaccines Can Eliminate Cervical Cancer
Cervical cancer is the fourth most common cancer in women, with around 660,000 new cases diagnosed globally each year and approximately 350,000 annual deaths. This burden is concentrated in low- and middle-income countries (LMICs) as a result of limited access to prevention, screening, and treatment services. Women living with HIV are also at an increased risk for developing cervical cancer due to their lowered ability to fight off infections.
As nearly all cases of cervical cancer are attributable to HPV infection, HPV vaccination is a proven strategy to decrease the burden of cervical cancer around the globe. HPV vaccines have been found to have close to 100% efficacy for preventing vaccine-type persistent HPV infection. As such, HPV vaccination is a pivotal component of the World Health Organization (WHO) global strategy to accelerate the elimination of cervical cancer as a public health problem. By 2030, the strategy aims to vaccinate 90% of girls with HPV vaccine by the time they turn 15 years old. Modelling estimates demonstrate that reaching this target—along with increases in screening and treatment—could help to reduce cervical cancer incidence by up to 97% by 2120, equal to 74 million cases and over 62 million deaths averted in the same time period. In the short-term, we have already seen a significant decrease in cervical cancer-related deaths in the United States, the first country to introduce HPV vaccines in 2006. HPV vaccination has also been shown to decrease the risk of head and neck cancer among boys and men, indicating the wide-reaching impact of these vaccines as cancer prevention tools.
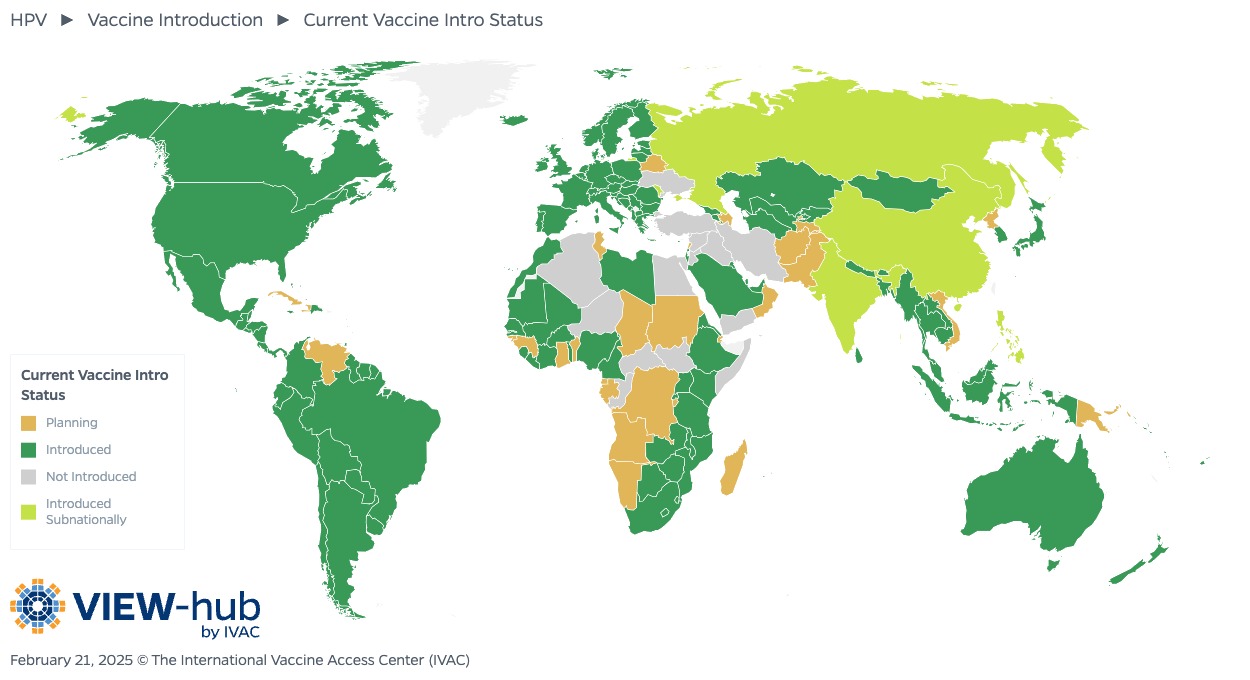
To optimize HPV immunization, we need to ensure that adolescents everywhere have access to these vaccines. As of February 2025, 48 countries have yet to introduce HPV vaccines into their national immunization programs. In countries that have introduced national HPV vaccination, coverage remains far below targets. To accelerate vaccine introduction, improve coverage, and increase equity, countries can consider alternative vaccine schedules. For example, the single-dose schedule included in WHO’s most recent recommendations—adopted so far by 67 countries—could help to address financial or logistical barriers to effective vaccine delivery. Integrating HPV vaccination with other adolescent health services is another approach to increase program sustainability and increase coverage, particularly among vulnerable populations.
HBV Vaccines Can Prevent Liver Cancer
Nearly 300 million people live with chronic HBV infection, the most common risk factor for developing liver cancer. Those living with HIV are especially at-risk, with approximately 10% of the global HIV-infected population also infected with HBV.
HBV vaccination has led to a significant decrease in transmission of HBV with a subsequent decrease in liver cancer. One modelling study estimates that HBV vaccination will avert 38 million deaths among those born in 98 LMICs between 2000 and 2030. As infants and children who become infected with the virus are most likely to develop chronic HBV, the WHO recommends that all babies receive their first dose of HBV vaccine within 24 hours of birth. However, many countries have not yet introduced universal birth dose vaccination. As of May 2024, only 15 out of 47 countries in the WHO African Region had included birth dose HBV vaccination in their routine immunization programs, leaving nearly 28 million children vulnerable to HBV.
Efforts to increase HBV vaccination access and coverage should focus on the introduction of universal birth dose HBV vaccination in all countries, strategies to reach children born outside of health facilities, and more effective delivery of subsequent doses to ensure that all children are fully protected against infection. In addition to ensuring and broadening access to HBV vaccination, development of a vaccine for hepatitis C is also critical to reducing liver cancer burden.
Related Resources
- [BRIEF] Understanding Priorities and Needs for HPV Vaccine Advocacy: Findings from a Global Survey
- [NEWS STORY] One Dose at a Time: Mobilizing to Eliminate Cervical Cancer in Nigeria
- [WEBINAR] Decision-Making Considerations and Drivers of Country-Level Adoption or Switch to a Single-Dose HPV Vaccination Schedule


