Lancet Series Launch: The Current and Future Outlook for Primary Health Care in South Asia
Noncommunicable Diseases, Urban Health, and Community Health Worker Roles Play Key Roles, New Lancet Series Finds

A new series published August 20, 2024 in The Lancet Global Health and The Lancet Regional Health Southeast Asia presents recommendations for improving primary health care in five South Asian countries: Bangladesh, India, Nepal, Pakistan, and Sri Lanka. At a Lancet launch event on October 1 at 9 a.m. EDT, study authors will discuss their recommendations and explore what they learned through the analysis of primary health program implementation in those countries.
The series is edited by Krishna D. Rao, PhD ‘04, MSc, associate professor in the Department of International Health at the Johns Hopkins Bloomberg School of Public Health
South Asian countries face many common health challenges due to noncommunicable diseases, population aging, rapid urbanization, socioeconomic inequalities, and low public spending on health. Improving and expanding primary health care’s role in health systems can serve as a cost-effective strategy in addressing these challenges in South Asia and other low- and middle-income countries.
The series offers nine action items for policy- and decision-makers to reorient health systems towards primary health care:
- Contextualize policies on primary health care.
- Scale up innovations.
- Allocate adequate financial resources.
- Strengthen the governance function of health ministries.
- Establish meaningful public-private engagements.
- Use digital health tools.
- Reorganize service delivery.
- Enable effective change-management processes.
- Encourage practice-oriented research.
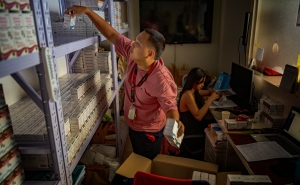
Major themes emerging from the series include the growing burden of noncommunicable diseases, which disproportionately impacts marginalized populations; the growth in urban populations, resulting in socio-economic inequalities and health disparities; and the key role community health workers play in improving population health and the importance of investing in them.
Noncommunicable diseases: The region has a high burden of noncommunicable diseases, such as heart disease, diabetes, cancer, and respiratory illnesses, as well as a high rate of modifiable risk factors, such as tobacco and alcohol use, unhealthy diet, and lack of physical activity. While there is political commitment to address NCDs across the region, there are challenges in doing so, such as shortages of human resources and essential medicines for NCDs, as well as a lack of dedicated financing. Authors emphasize integrating NCDs into the primary care system by implementing early detection of NCDs at the primary care level, dedicating funding for uninterrupted supplies of essential NCD medicines and technologies that can be delivered at primary care facilities, and developing the capacity of health workers to care for NCDs.
Urban health: South Asia is rapidly urbanizing. Cities often find it challenging to provide quality health care and healthy living and working conditions to all residents. Large inequalities in health characterize the region’s cities. Addressing these challenges through primary health care requires a multi-sectoral response with effectively resourced urban local bodies, such as those in housing and sanitization, and increased public financing for health care. “Policies should ensure quality services and financial protection through expansion of public sector services and strategic engagement with private providers, particularly those serving low-income urban populations,” says Rao.
Community health workers: Community health workers are the backbone of primary health care service delivery. South Asia’s current and future health challenges require further adaptations of community health worker (CHW) programs. Yet, in many South Asian countries, CHWs are not formalized within the health systems and not treated or paid adequately as professional health workers. Strengthening CHWs programs in South Asia requires adequate, dedicated, and consistent public funding; supporting career pathways that foster professional development; providing greater clarity of roles and responsibilities; and better integration into the health workforce.