World Mental Health Day: Mental Health is a Universal Human Right
How seven researchers are addressing mental health care as a human right.

The theme of this year’s World Mental Health Day is “mental health is a universal human right.”
The Bloomberg School is the only school of public health with a dedicated department of mental health. Researchers in this department as well as several others work every day to advance mental health care as a human right.
Here’s how seven researchers across the School are working to improve mental health care—whether by expanding access to care, addressing discrimination, developing novel interventions, or building on community strengths—in settings around the world.
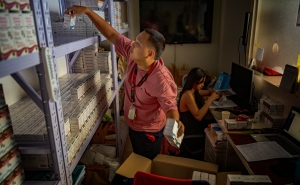
Integrating Mental Health Care Into Medical Care
Pamela Y. Collins, MD
What I’m doing: My colleagues and I work to meet the mental health needs of people at risk for and living with HIV in countries around the world. We’ve done this by:
- Introducing evidence-based psychological care into routine HIV care.
- Bringing mental health specialists to care for people living with HIV and depression.
- Working with UNAIDS to help programs integrate mental health and HIV care.
- By designing research to help us learn how to improve the delivery of care in HIV settings.
The social conditions that create risk for HIV also create risk for mental health conditions, often increasing their prevalence among people living with HIV. Access to compassionate mental health care is essential.
How my work encapsulates “mental health as a human right”:
The majority of people with major depressive disorder do not receive care. A recent study showed that among people with major depressive disorder in high-income countries, only around 33% used mental health services and 23% received minimally adequate treatment. In lower middle-income countries, these figures are much lower: 8% and 3.3%, respectively.
As a global community, we must ensure that people have access to community and social supports that promote mental health and improve quality of life. And for people experiencing distress or more serious symptoms, increasing access to care and services is a priority.
One game-changing innovation in the works:
The World Health Organization’s Special Initiative for Mental Health is working to transform access to mental health services in places like Ukraine, Zimbabwe, Paraguay, and Jordan. The nine countries initially participating are shaping their plans for scaling up care according to population needs and major drivers of well-being such as war, HIV, and climate events.
A significant need in all of these settings is the integration of mental health care into medical and community platforms. The good news is that this is happening as international and domestic funders better understand the importance of offering holistic care for multiple needs and appreciate how to use evidence to do so.
Leveraging Indigenous Traditions For Culturally Informed Care
Victoria M. O'Keefe, PhD
International Health, Center for Indigenous Health
What I’m doing: I’m work with American Indian and Alaska Native communities using community-based participatory research and Indigenous research methodologies to focus on strengths-based and culturally informed suicide prevention, mental health promotion, and wellness. Some of the projects include:
- Our Smallest Warriors, Our Strongest Medicine: Overcoming COVID-19
- Our Smallest Warriors, Our Strongest Medicine: Honoring Our Teachings During COVID-19
- The Elders Resilience Curriculum (Nohwi nalza dayúwéh bee goldoh dolee)
One game-changing innovation in the works: Indigenous communities and researchers are innovative in carrying out community-based participatory research (CBPR) and Indigenous research methodologies that privilege local knowledge, values, and traditions within mental health research and programming.
Aligning with CBPR, I enjoy working with our project teams to develop creative ways to disseminate mental health education and research within communities through projects like storybooks, videos, and infographics.
Inclusion and Lived Experience to Improve Service Delivery
Judith K. Bass, PhD
Mental Health, Center for Global Health, Center for Humanitarian Health
What I’m doing: I have spent my career identifying what interventions work for different populations and problems around the world. My focus has been on figuring out who needs what program, and where and how it should be provided.
Now that we have a lot more evidence on what interventions and programs can work, I have shifted my efforts to figuring out how we build systems that help sustain effective programs and ensure they continue to evolve to meet the local population’s changing needs.
How my work encapsulates “mental health as a human right”: I want to home in on the term “universal.” Too often, our research and public health programs have not involved all members of a population. Too many people have been left out, due to marginalization, disconnection, stigma, and other social and structural factors. The “universal” theme is a reminder that to truly improve population mental health, we need to be intentional with inclusion.
One game-changing innovation in the works: While not really new, the movement to increasingly include people with lived experience in mental health service delivery—through peer provider programs and partnerships for program planning, implementation, and ongoing monitoring—will truly improve what and how services are implemented around the world.
Destigmatizing Mental Health Care and Advocating for Equal Rights for Those Affected
Paul Anthony Bolton, MBBS
Mental Health, Center for Humanitarian Health
What I’m doing: I focus on global mental health advocacy and aim to reduce the stigma and discrimination of people with mental health problems.
Stigma and discrimination are practically universal. People with mental health problems feel pressure from the law, their families, and society to stay silent, which results in a largely invisible population whose issues are not being addressed. People with severe mental illness also run a risk of long-term incarceration in institutions that, in most countries, provide poor treatment for people with mental illness, isolating them from society.
How my work encapsulates “mental health as a human right”: Mental health, like physical health, is a human right. But it gets little attention and even fewer resources in comparison. According to WHO, mental health problems cause 14% of morbidity and 14% of global mortality and yet typically receive less than 2% of government health budgets—two-thirds of which goes to psychiatric hospitals that incarcerate patients for years or decades. The result is almost no community-based mental health services of the type that are required for real access to care.
Additionally, all over the world, society accepts violations of the rights of people with mental illness. Most countries allow for prolonged and arbitrary detention. More than a third of UN countries do not allow people with mental health conditions to marry or vote, and a quarter allow discrimination in employment. The cumulative effect is that people with mental health problems are treated as second class citizens by their governments and communities.
Critical parts of my work include creating awareness of this reality, engaging with governments and organizations to reverse it, and forming partnerships to address these issues.
One game-changing innovation in the works: Most people with mental health problems can be substantially helped through counseling that offers general support, simple coping strategies, or psychotherapy. These interventions can be provided by local, nonprofessional people if given adequate training and supervision. Apps, smartphones, and virtual meeting places allow us to deliver these services across large distances and, critically, across borders and into conflict zones and other insecure areas. In the future, counseling-based mental health interventions could be the most universally available of all health interventions.
Investigating the Double-Edged Sword of Technology
Johannes Thrul, PhD
What I’m doing: My research interests focus on the intersection between technology, substance use, and mental health. I investigate both how technology can be used to improve mental health and substance use outcomes, as well as how digital technology itself, if overused, can become a problem for individuals—for example, problematic use of the internet, including social media and online games.
How my work encapsulates “mental health as a human right”: Everyone deserves to live a life that is free from harmful industry influence. Unfortunately, the incentives for some industries are to make money at the expense of their customers’ health. This is especially a problem when considering addictive products, for example tobacco, alcohol, and, increasingly, social media and other technologies. When the profit motives of the industry and the health of the customer are directly at odds, it is our responsibility as public health researchers to address this problem.
One game-changing innovation in the works: I’m excited about the potential of digital and mobile health applications to improve mental health outcomes. We can learn a lot about someone’s unique mental health challenges by collecting self reports and sensor data via smartphone. We can then use this information to develop and deliver highly tailored treatments, including messages that recommend coping strategies when someone really needs support. Together with professional and peer support, these interventions will hopefully make big contributions toward improving mental health in the future.
Preventing Suicide In Latine Youth
Kiara Álvarez, PhD
What I’m doing: My research focuses on three intersecting areas: youth suicide prevention, mental health equity, and the well-being of Latine and immigrant youth and families. Several of my projects focus on identifying how community health workers can advance suicide prevention for Latine youth, including through support to parents in pediatric primary care and through delivery of prevention programming in community settings. I’ve also focused more broadly on the structural context of youth suicide prevention, including the impact of structural racism on systems of care for youth of color.
How my work encapsulates “mental health as a human right”: This theme underscores the ultimate goal of mental health equity work: to dismantle unjust systems and move toward a world in which all people can thrive. It also echoes other universal human rights; we could alleviate many mental health impacts on youth if we genuinely provided for their universal rights, as defined by the United Nations, to health, education, care, protection, shelter, and freedom from violence, abuse, and discrimination.
One game-changing innovation in the works: The expansion of the mental health workforce to include lay or community health workers, who share experiences similar to the communities they serve, has had immense impact internationally and increasingly in many communities in the U.S. If we can create sustainable and equitable pathways for community health workers to be a permanent part of our mental health workforce, working alongside other specialties, we can move toward more opportunity for optimal mental health for all.
Addressing Mental Health Disparities for People With Disabilities
Heather E. Volk, PhD
Mental Health, Environmental Health and Engineering, Epidemiology, Wendy Klag Center for Autism and Developmental Disabilities
What I’m doing: My research seeks to identify environmental and genetic factors that influence neurodevelopmental outcomes, including autism spectrum disorder. I study how inherited influences and those from the environment can impact both the developing brain and behavior.
How my work encapsulates “mental health as a human right”: Just recently, people with disabilities were designated by the National Institute on Minority Health and Health Disparities as a population with health disparities. The work I do seeks to improve the quality of life for individuals with disabilities as well as their families and caregivers. We further recognize that individuals experience a range of impairment, and that all such voices can contribute to our research goals.
One game-changing innovation in the works: I think the growing intersection of neuroscience and public health will change the understanding and scope of mental health research. Many large national efforts underway that are built on neuroscience initiatives allow for incorporation of the social, chemical, physical, and even in utero environment. Public health tools, which enable the rigorous study of these factors, when combined with an understanding of the brain itself, will provide new insights into behavior, its underlying mechanisms, and targets for intervention and support.