Editing Out Malaria, One Mosquito at a Time
Rendering mosquitoes incapable of transmitting human pathogens could be the key to eliminating malaria.
According to the WHO, in 2020 there were an estimated 241 million new cases of malaria and 627,000 malaria-related deaths in 85 countries. Current approaches to disease control like bed nets, drugs, and insecticides are effective, but logistically and financially difficult to maintain. But what if the mosquitoes could never get infected in the first place?
In this Q&A, adapted from the April 25 episode of Public Health On Call, George Dimopoulos, PhD, MBA, of the Johns Hopkins Malaria Research Institute talks with Stephanie Desmon about his lab’s research in creating genetically modified plasmodium-resistant mosquitoes, as well as existing approaches to controlling and ending malaria.
What causes malaria, and how is it transmitted?
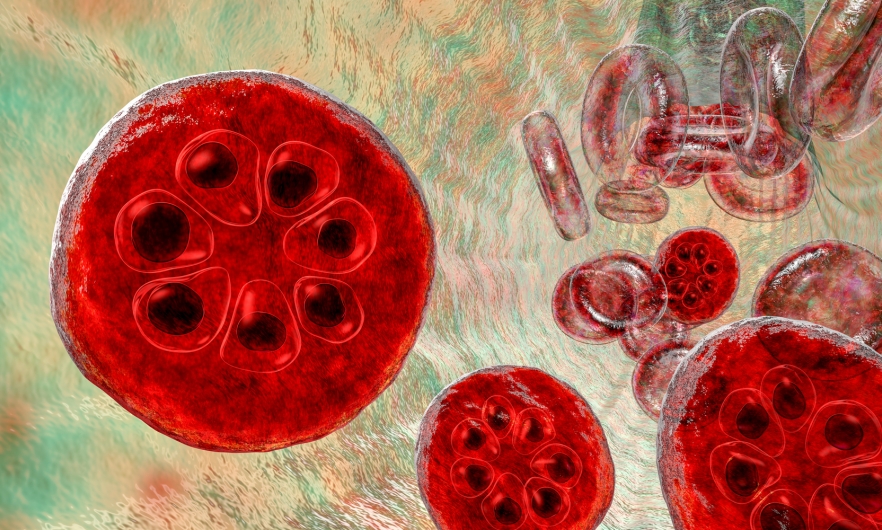
Malaria is a disease caused by the pathogen Plasmodium. It is transmitted between humans through mosquitoes. When a hungry female mosquito feeds on blood from a malaria-infected human, it will also become infected with the malaria parasite. That parasite will then develop in the mosquito—the development into an infectious stage will take about two weeks. At that time, the mosquito may want to feed again, and when it feeds on another human, it will pass on that infectious stage of the parasite. That is how malaria is transmitted.
What is the scope of the problem of malaria? How have we gotten where we are today?
Malaria has been with us for a very long time. The first descriptions of malaria are found in ancient Chinese medical records from 2700 BCE. In the 16th century, the Spanish started to use tree bark to treat malaria, and in 1820, a French chemist identified the first drug for malaria. We started to use chemicals to control malaria almost 100 years ago, and, despite that, we still have malaria, and it's a serious problem. There are about 228 million cases and approximately 600,000 deaths a year. Ninety percent of cases and deaths occur in Africa. Half of the world's population is at risk for malaria because of the prevalence of mosquitoes in those areas.
The major challenges to controlling malaria are the parasite’s ability to develop resistance to malaria drugs, and the mosquito’s ability to develop resistance to insecticides. All the current and past strategies [to control the disease] require a continuous effort that is very costly and logistically complicated. [Insecticide] spraying, taking drugs, removing mosquito breeding sites, using bed nets, etc., requires a continuous effort and the compliance of people who live in malaria-endemic areas.
But your lab is trying a different tack by trying to genetically modify the mosquitoes so that they no longer can get the parasite.
That's right. We are focusing on curing the mosquito rather than curing the human. We know that the parasite has to go through a complicated life cycle in the mosquito in order to become transmitted to a human host. There are many different ways by which we can interfere with that life cycle of the parasite in the mosquito and block it.
The mosquito has an immune system like us, [but] it's simpler. It's more primitive. It's called an innate immune system, and [it fights] the malaria parasite, but it is not sufficiently effective to kill all the parasites that the mosquito will acquire. We have found ways to genetically engineer the mosquito’s immune system to make it stronger and better at killing the parasite.
The long-term goal of our project is to develop mosquitoes that are resistant to the malaria parasite through genetic engineering of specific genes that [then] spread these resistance traits in natural mosquito populations. Eventually, all the mosquitoes would become resistant to the parasite and would not be able to transmit it.
The main advantage of this strategy is that no one has to do anything in terms of effort and compliance in using bed nets, spraying insecticides, or taking drugs. It's also an egalitarian approach: Everyone gets protected, not only those who can afford the drugs or have access to the bed nets. Those are the main advantages of this approach that we think could become a game changer in the fight against malaria.
How far away are we from testing this?
Testing has already started in the laboratory. We have to do extensive testing of different strains of mosquitoes that have been engineered in different ways to block the parasite. Before we can even consider testing in nature, we have to make sure that these mosquitoes are as fit as natural mosquitoes, so they can actually compete with them. We have to make sure that the parasite can't develop resistance to the engineered blocking mechanism. We will have to make sure that the engineering that we do to the mosquito does not have any negative impact on ecology or the food chain, cause a more severe bite reaction in humans, [or allow mosquitoes to] transmit another pathogen easier. I predict that we are about four to six years away from field trials.
While this all sounds wonderful, folks out in the field are more reluctant.
I wouldn't say that the majority [of folks] in the field are not super excited. There is a concern with regard to genetic engineering of organisms in general. We are approaching this problem in a way that ensures that the engineering of these mosquitoes is not going to lead to any unpredictable adverse results. One good thing about gene drive is that you can also reverse it. If something went wrong, you could release another gene-driven mosquito and cancel out the first one. So, there are mitigation strategies in place.
There will be thorough testing in the field before we can even consider using this technology for malaria control. It may take many years before we can actually roll out and implement the strategy. Some people may find that discouraging, but I think it's more important to come up with a long-term effective solution to this problem than trying to make shortcuts and looking for quick and short-term solutions. We have seen many examples of that in the area of malaria.
This has been attempted in the U.S. for a different kind of mosquito for other diseases. What was the result?
The technology that has been used in the United States is different from what we are looking at implementing. There are two basic gene drive technologies that one can use for malaria control. The technology we are developing is to render mosquitoes resistant to the parasite and then spread that resistance into the mosquito population. You're not getting rid of mosquitoes; you're just replacing mosquitoes that can transmit malaria with other mosquitoes that can’t.
The strategy that has been tested in the U.S. was performed with a mosquito species that does not transmit malaria—because there's no malaria in the U.S.—but does transmit arboviruses such as dengue and Zika, which do occur in the U.S. In this strategy, large numbers of mosquitoes are reared in facilities, engineered to be sterile, and then released in nature. Because they're sterile, when they mate with the natural mosquitoes, they don't produce any offspring. By suppressing the population, you significantly decrease the number of mosquitoes in a certain area. That technology is powerful, and there is probably a lesser concern with the genetic engineering component there because the engineered gene does not persist in nature because those mosquitoes die. They don't pass that mutation on to the offspring.
But the problem with that technology is that it's expensive and logistically complicated. You need to release these mosquitoes continuously, in very large numbers, and if you stop releasing them for a certain period of time, that area is going to become repopulated with new mosquitoes from other parts of that geographic region, resulting in the resumption of disease transmission.
Stephanie Desmon is the co-host of the Public Health On Call podcast. She is the director of public relations and marketing for the Johns Hopkins Center for Communication Programs, the largest center at the Johns Hopkins Bloomberg School of Public Health.
RELATED:
More from the Bloomberg School
- See latest headlines
- Learn more about our departments: