Dangerous Curve: Predicting the Coronavirus Peak
The image is ubiquitous on social media: a line graph with a sharp, high peak on the left and a broad, much lower peak on the right, accompanied by admonitions to “flatten the curve” for novel coronavirus infections.
What will the peak look like for COVID-19 in the U.S.? And when will it occur?
“Those are hard questions to answer,” says Caitlin Rivers, PhD, MPH, a senior associate in the Johns Hopkins Center for Health Security and an assistant professor in Environmental Health and Engineering at the Bloomberg School. “We usually don’t know that we’ve reached the peak until we’re past it. And at this point, we don’t know what the next day will bring,” she says.
Rivers points out that measures meant to stem transmission in the U.S., such as school closures and recommendations for social distancing, were only relatively recently put into place. If those interventions do what they’re supposed to, then the number of new cases should gradually slow and then stop as they have in other hard-hit locations. For example, in Hubei, China—the province where the disease was first identified and spread like wildfire before the government instituted a strict lockdown—new cases have slowed to a trickle in the past week.
But it may be much harder to impose that kind of lockdown across the U.S., where personal freedom is part of the culture, says Shaun Truelove, PhD, MPH, an assistant scientist in International Health. Spotty implementation of largely unenforceable interventions across different states make predicting when the peak will occur more difficult; so does the paucity of data available on the actual rate of newly diagnosed cases due to limited testing. “We are probably only catching a small fraction of those who are sick, making it a challenge to predict what will happen next,” he says.
With such sparse data, statistical models used to forecast the path of other infectious diseases is only partly useful here, explains Thomas McAndrew, PhD, a postdoctoral fellow in the Department of Biostatistics at the University of Massachusetts at Amherst. That’s why he and his mentor, associate professor of Biostatistics Nicholas Reich, PhD, recently started sending out weekly forecasting surveys to a variety of COVID-19 experts with different backgrounds: infectious disease modelers, physicians in the field, epidemiologists, and others.
Right now, he says, these experts are predicting a peak in the number of hospitalizations in May, with a strong possibility of a second peak sometime this fall.
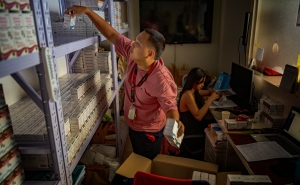
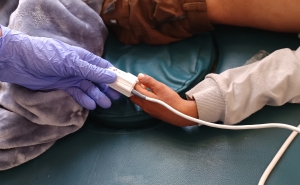
Justin Lessler, associate professor in Epidemiology at the Bloomberg School, says that whenever the peak actually occurs, we’re likely to see increasingly more of what’s already occurring: overstressed health care systems short of beds and personal protective equipment that put all patients—not just those infected with the virus—at risk.
“Right now, we’re aiming for a completely different scenario than the two peaks presented in that social media graph,” he says. “We’re aiming to knock it down altogether.”
RELATED CONTENT
More from the Bloomberg School
- See latest headlines
- Learn more about our departments: