5 Ways the U.S. Botched the Response to COVID-19
BY JULIE SCHARPER
On March 25, the U.S. hit a grim milestone: With more than 83,000 people diagnosed with COVID-19, it had become the nation with the highest number of confirmed cases.
The next day, the number of cases soared past 100,000. By April 1, that figure had more than doubled.
Officials had been aware of COVID-19’s virulence since early January. Yet despite widespread reports of the devastation the virus wreaked in China, Italy, and Iran, the U.S. seemed caught unprepared by the virus. What went wrong?
Widespread testing was delayed and remains inadequate
On January 20, the first cases of COVID-19 were identified in both the U.S. and South Korea. But while South Korea rapidly began to test 10,000 people per day and isolate infected people, the U.S. was slow to begin testing.
The CDC eschewed a test created by the World Health Organization, instead creating on their own test—which turned out to be flawed, causing the loss of more valuable time. Access to testing remains limited in most areas.
“When we look back at this a generation from now, the failure to implement early and expansive testing will be seen as the crucial failure here,” says Jeffrey Schlegelmilch, deputy director for the National Center for Disaster Preparedness at Columbia University’s Earth Institute. “We missed the window where we could do really aggressive contact tracing and isolating.”
The U.S. was unable to contain the spread of the virus
Without comprehensive testing, U.S. officials found it difficult to gauge the spread of the virus and identify carriers. Throughout February and much of March, public health officials at all levels of government advised people to stay home if sick and practice good hand hygiene. Yet this advice failed to acknowledge that COVID-19 can be spread by inhaling microscopic droplets exhaled by an infected person, or that an infected person can spread the virus before showing symptoms. The virus spread widely in February and March; people got infected at parties, funerals, spring break trips, and even New Orleans’ Mardi Gras celebrations.
“We saw lots of different actions happening across the country, but broadly we weren’t quick enough in our response to the pandemic,” says Meghan McGinty, PhD ’16, MBA/MPH ’08, a faculty associate in Health Policy and Management at the Bloomberg School.
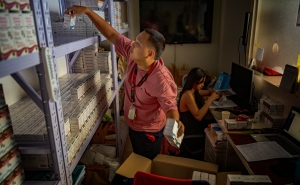
The country lacks essential supplies and equipment
For decades, says Thomas A. Burke, PhD, MPH, associate chair of Health Policy and Management, public health leaders have sounded alarms that the Strategic National Stockpile did not have enough masks, personal protective gear, and ventilators to face a pandemic. Recent reports indicate that this stockpile is nearly depleted.
When news of the virus reached this country, the federal government should have taken prompt action to obtain supplies and equipment, Burke says, but that did not happen. “Imagine if we had those two months back,” he says. “We could get those masks made and get the respirators we need.”
Messaging on the virus has been inconsistent and inaccurate
Through much of February, President Trump downplayed the severity of the crisis, saying that the few cases in the U.S. would soon be brought down to zero. As recently as March 9, he compared COVID-19 to the flu. In late March, he declared that social distancing measures would be relaxed by Easter; a few days later, he acknowledged they would need to continue through at least the end of April.
“The seriousness of the threat, and the importance of containing it, should have been communicated early and clearly,” says Sandra C. Quinn, chair of the Department of Family Health at the University of Maryland’s School of Public Health. “We need to be hearing blunt talk mixed with empathy,” she says. “We hear that from some of our governors, but we do not hear that from the White House.”
Federal and state agencies failed to coordinate their efforts
Much of the public health authority in the U.S. lies not at the federal level, but within the country’s more than 2,000 state and local governments, says Lainie Rutkow, PhD ’09, JD, MPH ’05, a professor in Health Policy and Management. While the CDC recommends courses of action for local governments, these are framed as guidance and do not carry the force of law.
The way a jurisdiction responds to a health crisis depends on local politics, funding, and the culture of that area. “Some states have done extensive planning and preparedness; others have been less inclined to do that,” says Rutkow. There’s even great variation among counties and municipalities within a single state. One jurisdiction might take a proactive approach to controlling the virus, only to see its hospitals overburdened by people from a neighboring jurisdiction that failed to contain it.
So how can future public health crises be prevented?
For one thing, says Quinn, it's important to maintain consistent funding for public health preparedness planning. "When the problem goes away, the funding goes away," she says.
Moreover, U.S. public health policy must be guided by science, including recommendations offered in the Global Health Security Index.
“I hope this is a big wake up call,” says Burke. “We’re all in this together, and we need to reinvest in our health care system and our public health system.”
Julie Scharper is a writer based in Baltimore. Her work has appeared in the Baltimore Sun, the Washington Post, the New York Times, Johns Hopkins Magazine, and Hopkins Bloomberg Public Health.